Welcome to MBC Biology!
In this post, I'm presenting you concise description Connective Tissues.
Some
tissues bind different types of cells or tissues together in an organ, called connective
tissues. They are major supporting tissues of the body. They develop from
the mesoderm. These tissues constitute about 30% of the body.
Structure of
connective tissue
Basically,
three components – cells, fibres, and matrix – constitute
a connective tissue.
1. Cell
Cells
are living components of connective tissues. These are widely distributed in
the matrix. The different types of cells are fibroblasts, macrophages
or histocytes, mast cells, and plasma cells.
Fibroblasts:
They are spindle shaped cells with long protoplasmic processes. They have oval
nucleus. They form fibres.
Macrophages
or histocytes: These are large irregular-shaped or amoeboid polymorphic
cells with a kidney-shaped nucleus. They are actively phagocytic cells.
Mast
cells: These are large oval-shaped cells that produce heparin and
histamine. Heparin prevents coagulation of blood and histamine causes
inflammation.
Plasma
cells: They are small, round or irregular cells produced by the division of
migratory lymphocytes. They produce antibodies that help in defence.
2. Fibres
Fibres
are the non-living products of the cells. They are widely distributed in the
matrix. They are collagen or white fibres, elastic
or yellow fibres, and reticulate fibres.
Collagen
or white fibres: These are the long unbranched and white fibres
containing collagen, a protein. They are present in groups or bundles
and are flexible but inelastic.
Elastic
or Yellow fibres: These are the long, branched and yellow fibres
containing a protein elastin. They are present singly and are flexible
and elastic.
Reticulate
fibres: These are very short, fine, thread-like fibres containing a reticulin
protein. They are interconnected to form a network or reticular fibres.
3. Matrix
Matrix
is a non-living, transparent fluid or semisolid intercellular fluid containing
various organic and inorganic substances.
 |
| Figure 14 Different types of cells and fibres in connective tissue |
Types of Connective tissues
Connective
tissues are categorized as connective tissue proper, supportive
connective tissues or skeletal tissues, and fluid
connective tissue.
I. Connective tissue proper
Connective
tissue proper consists of a jelly-like substance containing white collagen
fibres or yellow elastic fibres or both, together with the cells. These fibres
are formed by fibroblasts. Based on the softness, rigidity, and degree of
toughness, the connective tissue proper is divided as lose connective tissue
and dense connective tissue.
1. Loose connective tissue
Areolar
tissue and adipose tissue are grouped under loose connective tissue.
a. Areolar tissue
Areolar
tissue is the simplest and most widely distributed connective tissue in the
body. It consists of a jelly-like soft matrix having fibres. Fibres and
other cells in it are white collagen fibres (made of collagen protein), yellow
elastic fibre (made of elastin protein), fibrocytes (large flat
cells that make white and yellow fibres), macrophages (the
irregular-shaped cells with granules and are actively phagocytic to engulf
bacteria and other foreign bodies), and mast cells (produce heparin and
histamine; heparin is for the coagulation of plasma and histamine is for the
inflammation to cell at the time of infection).
Areolar
tissue acts as supporting and packing tissues. It also helps in combating
foreign toxins released by pathogenic organisms.
b. Adipose tissue
Adipose
tissue is the modified areolar tissue consists of a large number of fat cells
or adipocytes. It is also called fat tissue. Adipocytes are rounded or
polygonal with a thin layer of cytoplasm. The nucleus lies at one side due to
fat. Fibres are absent or reduced. It is present below the skin (subcutaneous
fat), between internal organs (visceral fat) and in the inner cavities of bones
(bone marrow adipose tissue).
Adipose tissue serves as an insulating layer
against heat loss. It is a fat reservoir. It acts as cushion in the orbits or
eye sockets so that it prevents the eye from injury.
2. Dense connective tissue proper
White
fibrous tissue (tendon) and yellow elastic tissue(ligament) come under dense
connective tissue proper.
a. White fibrous tissue (tendon)
White
fibrous tissue is a modified areolar tissue consists of thickly packed white
collagen fibres. The fibres are tough and non-elastic. The fibres run parallel
to one another and form tendons. Tendons connect muscles with the
bones. Its matrix contains fibroblasts which are arranged between the rows
of the fibres.
White
fibrous tissue provides mechanical protection against stretch.
b. Yellow elastic tissue (ligament)
Yellow
elastic tissue consists mainly of thick and branched yellow elastic fibres.
Sometimes, white fibres are present. The matrix contains scattered fibrocytes.
Yellow elastic tissues may form the ligament which binds one bone with
another bone.
Yellow
elastic tissue provides stretch and elasticity.
 |
| Figure 15 Different tissues of connective tissue proper |
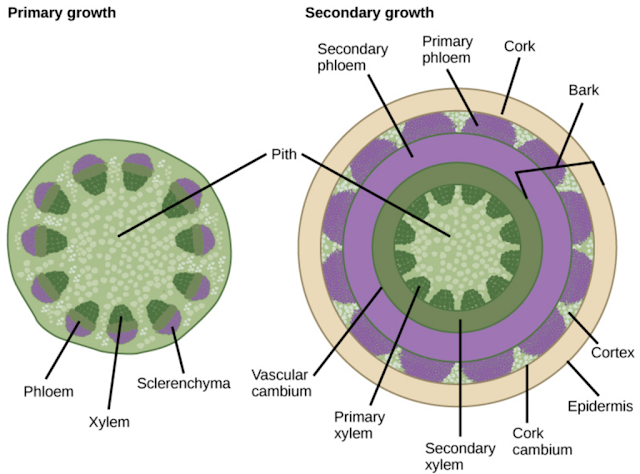
II. Supportive connective tissue or skeletal tissues
Supportive
connective tissue forms the endoskeleton of the vertebrates. It supports the
body and protects the delicate and vital organs from different injuries. These
tissues are cartilage and bone.
1. Cartilage
Cartilage
is the soft skeletal tissue in the vertebrates. A typical cartilage consists of
semi-solid matrix containing chondrin. This matrix is secreted by oval-shaped
small group of cartilage cells called chondroblasts or chondrocytes.
Chondrocytes are scattered in the matrix singly or in groups. They are enclosed
in the fluid filled spaces called lacunae. Cartilage is covered by
perichondrium, a thin and stiff membrane. The perichondrium produces and adds
new chondrocytes to the matrix.
Based
on the nature of matrix, cartilages are hyaline cartilage, elastic cartilage,
fibro-cartilage, and calcified cartilage.
Hyaline
cartilage: It is flexible. Its matrix is transparent, homogenous and tough.
It covers joint surfaces, endo of ribs, nose, and tracheal rings. It forms
skeletal cartilage in the embryos of all vertebrates.
Elastic
cartilage: It is more flexible. Its matrix consists of a network of
numerous yellow elastic fibres. It is found in the external ear (pinna),
external auditory canal of ear, epiglottis, eustachian tubes and tip of the
nose.
Fibro-cartilage:
Abundant white collagen fibres make its matrix. It is the most resistant
cartilage having less cells and matrix. It is found in the intervertebral discs
(pads) between the mammalian vertebrae and in the pubic symphysis around the
joints. In such places, it acts as cushion.
Calcified
cartilage: When the hyaline cartilage is impregnated with calcium in the
matrix, calcified cartilage is formed. It is a very hard, stiff and non-elastic
cartilage. It is found in the suprascapular of pectoral girdle, in the pelvis
of old frogs, in the heads of humerus and femur and in the vertebrae of sharks.
 |
| Figure 16 Different types of cartilages |
2. Bone
Bone
is specialized connective tissue. It is very hard due to the deposition of lime
(CaCO3) salts. It forms the two third of the skeleton of the body.
It provides a framework of the body. Its matrix has bone cells, called osteocytes.
Its matrix is formed by a protein called ossein. The matrix contains 70%
inorganic bone salts and 30% fibres and glycoprotein.
Structure of Bone
A
typical bone has periosteum, outer layer of osteoblast, endosteum,
matrix, and Haversian system.
Periosteum:
It is the outermost covering of bone. It consists of undifferentiated bone
cells.
Outer
layer of osteoblast: It lies just below the periosteum. These are flat
connective cells that give rise to the bone cells.
Endosteum:
It is a thin layer that covers the narrow cavity of the bone.
Matrix:
It covers the large part of the bone. It consists of various layers, called
lamellae. Each lamella has numerous small spaces, called lacunae.
Each lacunae encloses only one osteocyte. Each lacuna gives off branching
channels radiating in all directions, called canaliculi. These
canaliculi anastomose with other canaliculi forming an interconnected system in
the matrix, called Haversian system.
Haversian
system: It consists of lamellae arranged around the central canal, called Haversian
canal. Each canal with lamellae and canaliculi together forms a haversian
system. Many haversian systems are connected together by the canals of
Volkmann. It is found in the long bones.
Types of Bones
On
the basis of the type of matrix present, bones are classified as spongy bone
and compact bone.
Spongy
bone: Spongy bone is present on the expanded ends of the long bones. It is
filled with red bone marrow, a soft tissue. It lacks haversian system.
Compact
bone: It is present on the shaft of the long bones. It is filled with a
fatty tissue called yellow bone marrow. It has many haversian systems.
Bone marrow
The
bone contains two types of soft and spongy bone marrow – yellow bone marrow and
red bone marrow.
Yellow
bone marrow possesses high fat content and is mostly found in the long
bones.
Red
bone marrow is found in the short bones and on the surfaces of the long
bones. It produces RBC and WBC.
Ossification
Ossification
is the process of bone formation. It is of two types – endochondral and intramembranous
ossification.
Endochondral
ossification is the transformation of a cartilage into a bone. The bone
formed by such process is called cartilage bone or replacing bone.
Intramembranous
ossification is the formation of bone directly from the connective tissue.
The bone is called dermal investing or membrane bone.
 |
| Figure 17 Different structures in bone |
III. Fluid Connective Tissue (Haemopoitic Tissue)
Fluid
connective tissue consists of both myeloid and lymphoid tissues. Myeloid
tissues form blood while lymphoid tissues form lymph. They do not have fibres.
These tissues circulate in the body.
1. Blood
Blood
consists of plasma and corpuscles. A normal human adult contains 5 to 8 litres
of blood in the body. So, it constitutes 5-8 % of the body weight. It is
composed of blood plasma and blood corpuscles.
a. Blood plasma
Blood
plasma is a pale-yellow fluid. It forms 55% of blood by volume. It is slightly
alkaline. It contains various organic and inorganic materials. Its components
are water (90 to 92 %), dissolved solids (8 to 10%), proteins (7%; serum
albumin, serum globulin, and fibrinogen), organic constituents (1-2%;
nonprotein nitrogenous substances such as urea, ammonia, amino acids, neutral
fats, glucoses), respiratory gases (O2 and CO2), and internal secretions
(antibodies and various enzymes).
Functions of blood plasma
- Blood transports oxygen from the lungs to all the parts of the body and brings carbon dioxide from the tissues to the lungs.
- It transports soluble organic substances from the small intestine to the different parts of the body.
- It transports soluble excretory products from the tissues, in which they are produced, to the organs of excretion.
- It transports metabolic by-products from the areas of production to other parts of the body.
- It transports hormones from the glands to the target organs.
- It regulates the body temperatures and maintains the constant blood osmotic pressure and pH.
- It provides defense to the body against diseases by the phagocytosis, by the immune mediated by antibodies or lymphocytes, and by the clotting of the blood.
b. Blood corpuscles (cells)
The
three types of blood cells are erythrocytes or red blood corpuscles (RBCs),
leucocytes or white blood corpuscles (WBCs), and thrombocytes
or blood platelets.
i. Erythrocytes
Erythrocytes
are biconcave discs and non-nucleated but in fishes, frogs, reptiles, and
birds, they are oval and nucleated. They are 7.5 μm thick and are about
5,400,000 per mm3 of blood in men and about 4,800,000 in women. Their average lifespan in human is around
110-120 days. They contain red pigment the haemoglobin. They are formed in the red bone marrow by the
process of haemopoiesis. In foetus, they are formed in the liver and in
the spleen. They transport O2 and assist CO2 transport.
ii. Leucocytes
Leucocytes
are nucleated and non-pigmented cells. They have diameter of 8-20 μm and are
7,000-10,000 per mm3 of blood. They show amoeboid movement. They are produced
in the bone marrow and in the lymph glands. They normally live for 1-4 days
inside blood. The excessive blood formation is called leukemia, type of
blood cancer. They fight against infection by the process of phagocytosis.
Based
on the size, granules, staining reaction, number and shape of nuclei, WBCs are
classified as granulocytes and agranulocytes.
Granulocytes
Granulocytes
are with lobated nuclei and fine granules. They are formed from the red bone
marrow. They form 72% of total WBC. They are of three types – eosinophils
(acidophils), basophils, and neutrophils.
Eosinophils
(acidophils): These are the spherical cells having bilobed nucleus. They
are stained in acidic dyes. In human, they are with 9-12 μm diameter. They make
2-3% of total leucocytes. They mainly destroy and detoxify the toxins. The
excessive formation of eosinophils causes eosinophilia.
Basophils:
These are spherical cells with S-shaped nucleus. They are stained in basic
dyes. In human, they are with 9-12 μm diameter. They constitute 0.5-4% of WBCs.
They also release heparin and histamine.
Neutrophils:
These are spherical cells with multi-lobed nucleus. They are stained in neutral
dyes. In human, they are with 9-12 μm diameter. They constitute 60-70% of total
WBCs. The engulf bacteria or foreign bodies.
Agranulocytes
Agranulocytes
have oval nuclei without granules. They are formed in the red bone marrow and
lymph nodes. They form 28% of total WBCs. They are of two types – lymphocytes
and monocytes.
Lymphocytes:
They are small cells having large nuclei. In human, they are with 8-10 μm
diameter. They form 24% of total WBC. They are non-motile and non-phagocytic in
nature. They produce antibodies to destroy microorganisms. They are of
two types – B-lymphocytes and T-lymphocytes.
Monocytes:
They are large cells having nearly bean-shaped nuclei. In human, they are with
12-20 μm diameter. They form about 4% of total leucocytes. They are motile and
actively phagocytic in nature. They mainly engulf the microorganisms.
iii. Thrombocytes
Thrombocytes
are irregular and non-nucleated cells. They measure 2-4 μm of diameter. In
human blood, they are 250,000 per mm3 of blood. Their lifespan is
about 7 days. They help in blood clotting as they contain thromboplastin,
which speeds up the conversion of prothrombin to thrombin.
Function of blood
- Blood transports oxygen from the lungs to all the parts of the body and brings carbon dioxide from the tissues to the lungs.
- It transports soluble organic substances from the small intestine to the different parts of the body.
- It transports soluble excretory products from the tissues, in which they are produced, to the organs of excretion.
- It transports metabolic by-products from the areas of production to other parts of the body.
- It transports hormones from the glands to the target organs.
- It regulates the body temperatures and maintains the constant blood osmotic pressure and pH.
- It provides defense to the body against diseases by the phagocytosis, by the immune mediated by antibodies or lymphocytes, and by the clotting of the blood.
2. Lymph
Lymph
is the blood without RBCs, WBCs, and platelets. It is transparent, slightly
yellowish and alkaline fluid. It contains same concentration of glucose, salts,
amino acids, and vitamins as in plasma; less protein than in plasma. It
circulates throughout the body through lymph vessels and lymph hearts.
Functions of lymph
- Lymph is like a middle man and transports respiratory gases, food materials, hormones, etc.
- It produces lymphocytes and brings antibodies from lymph nodes to the blood.
- It destroys pathogens and foreign particles.
- Lacteals, the lymph capillaries in the intestinal villi, are associated with absorption and fat-soluble vitamins.
- It maintains the volume of the blood in the body. When the blood volume is reduced in the blood vascular system, the lymph rushes from lymphatic system to the blood vascular system to maintain the blood volume uniform.
 |
| Figure 18 Components of blood |